Background
The COVID-19 pandemic continues to challenge effective treatment delivery to hematologically-compromised patients, including those with myeloproliferative neoplasms (MPNs). MPNs are characterized by clonal proliferation of hematopoietic cell lines in bone marrow. As such, increasing reports of COVID-19 related thrombotic events highlight how MPN patients are at an increased risk in navigating potential complications during this pandemic. Mitigation strategies to lesson MPN patient exposure to COVID-19 are vital. Though, such efforts come at an inherent cost to effective healthcare delivery. Restriction of regular in-clinic treatments and reported shortages of MPN pharmacotherapies present these patients with diminishing continued care.
To understand how MPN patient care has been impacted by COVID-19, an internet-based questionnaire was deployed surveying a variety of disease and pandemic related items (reported elsewhere; Palmer J et al, ASH 2020 submitted). A single free-text response item instructed respondents to: "Please tell us anything else (bad or good) about how the COVID-19 outbreak has impacted your MPN care." This qualitative analysis evaluated first-hand comments directly from patients in order to form a richer understanding of how those with MPNs have been managing disease-related care amidst this pandemic.
Methods
This COVID-19 survey was hosted via Mayo Clinic's secured REDCap system for online surveys and posted on MPN organizational partner websites. Surveys were completely anonymous. The free-text responses describing impacts to MPN care were each independently reviewed by 2 individuals for overall sentiment (positive, negative, both, or neutral [no impact]) and categorized for themes. The 2 reviewers were assessed for agreement. Conflicting reviews were evaluated then adjudicated by an algorithm for cases meeting selected conditions or by lead author review for all remaining cases. Descriptive statistics are reported.
Results
Of the 1217 consenting adult patients participating in the overall COVID-19 study, 824 provided free-text responses. Of these, respondent MPN diagnoses included, essential thrombocythemia (n=324, 39%), polycythemia vera (n=251, 30%), myelofibrosis (n=153, 19%), and other/undisclosed (96, 12%); 69% (n=567) were female; median age was 63 (range 21-93); 38% (n=313) were from the US, 38% (n=313) UK, and 24% (n=198) other/unknown.
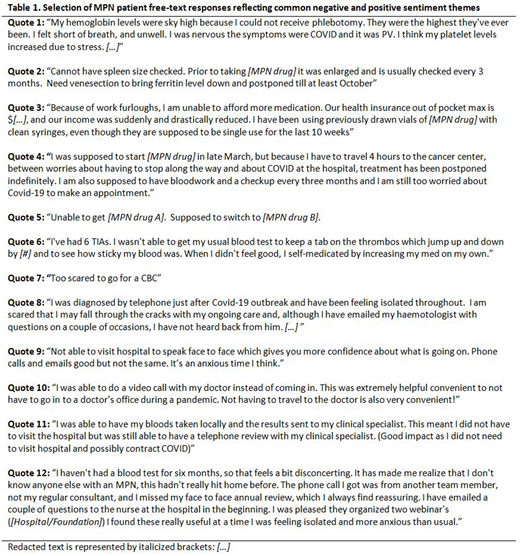
There was 89% (n=734) sentiment agreement between reviewers. Free-text responses about the impact of COVID-19 on MPN care were 49% (n=400) negative, 21% (n=177) positive, 8% (n=65) both positive and negative, and 22% (n=182) neutral/no impact. Table 1 shows a selection of MPN patient free-text responses reflecting common negative and positive sentiment themes.
Negative impact (n=400): The most common negative impact involved delays or cancellations of visits or perceived inaccessibility to regular providers (n=261, 65%). Primarily this sentiment was driven by lack of clinic availability and restrictions at treatment centers or by providers. However, some respondents reported delaying or canceling visits themselves due to fear of COVID-19 exposure. Perceived health consequences from this delay were also expressed. There were 129 (32%) respondents with concern regarding changes or access to medications, including explicit drug supply shortages. Some patients resorted to self-adjusting medications and reusing single-use supplies. General anxiety, stress, and isolation were also reported (n=98, 25%).
Positive impact (n=177): Availability of telemedicine comprised the majority of positive impacts of the pandemic (n=95, 54%), with many noting the reduced travel time to visits. Routine local testing coupled with follow-up telemedicine was favorable. Despite general positivity towards telemedicine, some reported preferences for in-person visits; commenting that telemedicine was impersonal, difficult to schedule or receive virtual communication, and expressed concern for lack of spleen examinations during virtual visits.
Conclusion
Positive and negative aspects were reported including MPN-specific issues. Healthcare systems should use such data to emerge from the COVID-19 pandemic and retain the positive impacts such as telemedicine, while developing education materials and other resources to address the reported negative impacts where possible.
Mesa:CTI BioPharma: Research Funding; Promedior: Research Funding; Novartis: Consultancy; Sierra Oncology: Consultancy; Samus Therapeutics: Research Funding; Genentech: Research Funding; AbbVie: Research Funding; Incyte: Research Funding; LaJolla Pharmaceutical Company: Consultancy; Bristol Myers Squibb: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal